Customer-Oriented Claims Management: The Claim As An Experience
Customer-Oriented Claims Management:
The Claim As An Experience
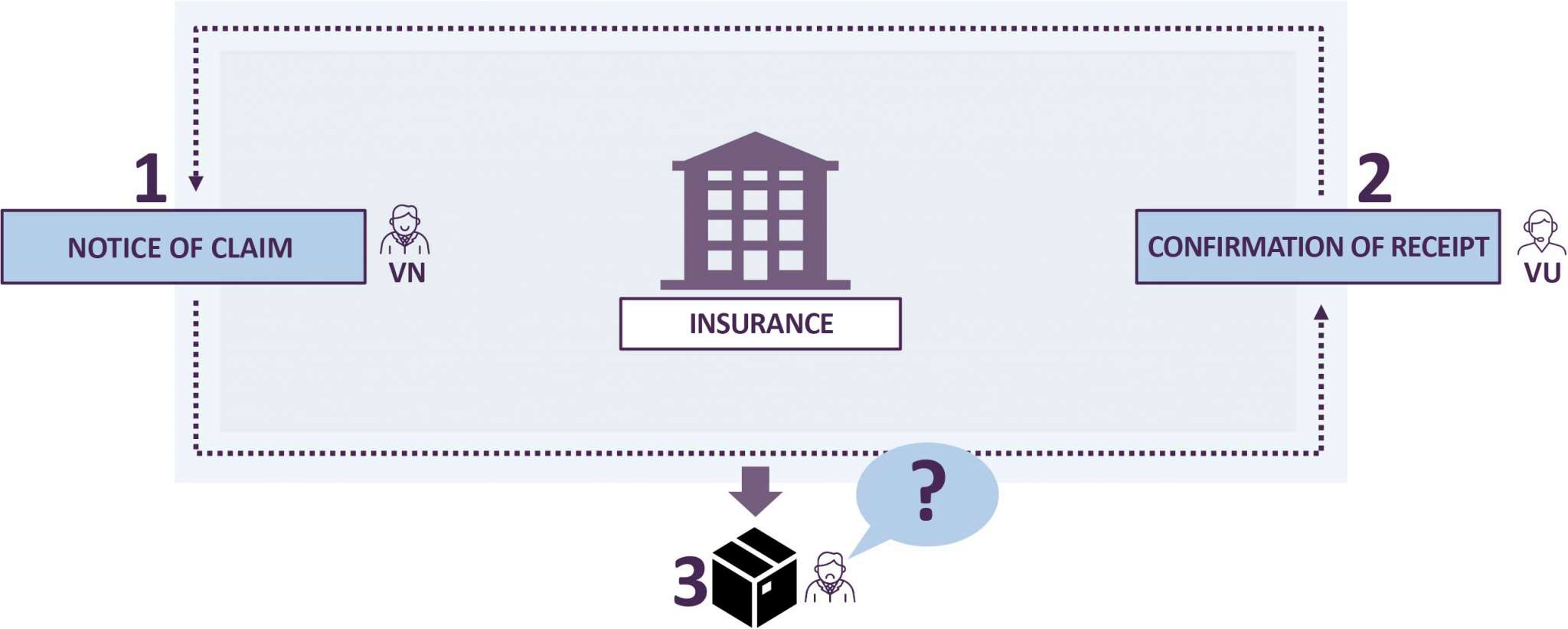
Over the course of a customer relationship, many insurance customers may ask themselves why they took out the insurance. It can be difficult for any individual policyholder to grasp the big picture of how insurance products mitigate risk across a variety of perils over time. The point of insurance is the promise of protection in the case of disaster. Policyholders need to know that if they make a legitimate claim, they can expect the policy benefits of their coverage. If the claim does occur, the promise of benefits should be realized. The point of insurance is the promise of protection in the case of disaster. Policyholders need to know that if they make a legitimate claim, they can expect the policy benefits of their coverage: Typically, at a high level, claims processes include the following steps: After damage occurs, policyholders report the incident and details to their insurance company, and receive confirmation that their claim has been received and an investigation has been opened. Eventually, they will receive notification of the findings and possibly reimbursement for their claim. But what happened in the meantime?! Why don’t policyholders receive status details as their claims proceeds through the various back-office process steps? This is a kind of black box at a time when customers need transparency and certainty to feel secure.
Nobody likes the feeling of not knowing whether the damage will actually be reimbursed. In recent years, the focus has been very much on topics of operational excellence (OPEX). This was partly at the expense of the customer experience, which is particularly important in the event of a claim. Insurers should create transparency here in order to align their claims management with customer orientation.
Customer management in the claims area
People love to have some form of control over their lives. This is not about mastering all the contents of life, but about holding the reins where one can make a difference. In those places that cannot be influenced, one wishes for at least some information or basic recommendations for action.
Many topics of everyday life have changed rapidly due to technical developments. For example, streaming services has become an entertainment that is always available on demand.
Like television a few years ago, insurance companies, as a supposedly untouchable good, are facing a comparable transformation. Customer needs will inevitably become increasingly important for the provider. It is true that insurers are already customer-centric when it comes to initiating and concluding contracts. However, when a loss occurs, where insurance benefits are effectively paid under the given circumstances, the customer’s involvement falls by the wayside. The customer suffers the damage, reports it and, in extreme cases, only learns of the settlement decision shortly before the conclusion of the claim.
Upon conclusion of the contract, the policyholder receives a sheet of paper (beautifully designed if necessary) on which a promise of insurance is formulated. In the event that these (abstractly and generically) formulated situations would occur, the customer will receive reimbursement of expenses, possible cost coverage and services. What this promise is worth is only revealed in an emergency – a loss. In this case, the insurer can make the customer very angry by not keeping his promise on the one hand, but on the other hand, keeping the promise offers the insurance company a great opportunity to inspire its own customers.
What if an experience was created in the event of an insured event (damage)?
Insurance: An experience?
No need to watch commercials on television anymore. See exactly what I want and when I want. This (possibly not dreamt) dream became reality. The most famous background noise of every family living area became an experience again.
For many insurers, a customer’s claim is often only an expense. Accordingly, it has always been important to minimize claims payments and benefit process costs. The extent to which the customer’s needs play a role in this is – if at all – a secondary consideration. A policyholder could experience the claim like a feature film. This triggers emotions similar to those of an insurance claim.
How can insurers make claims processing an experience?
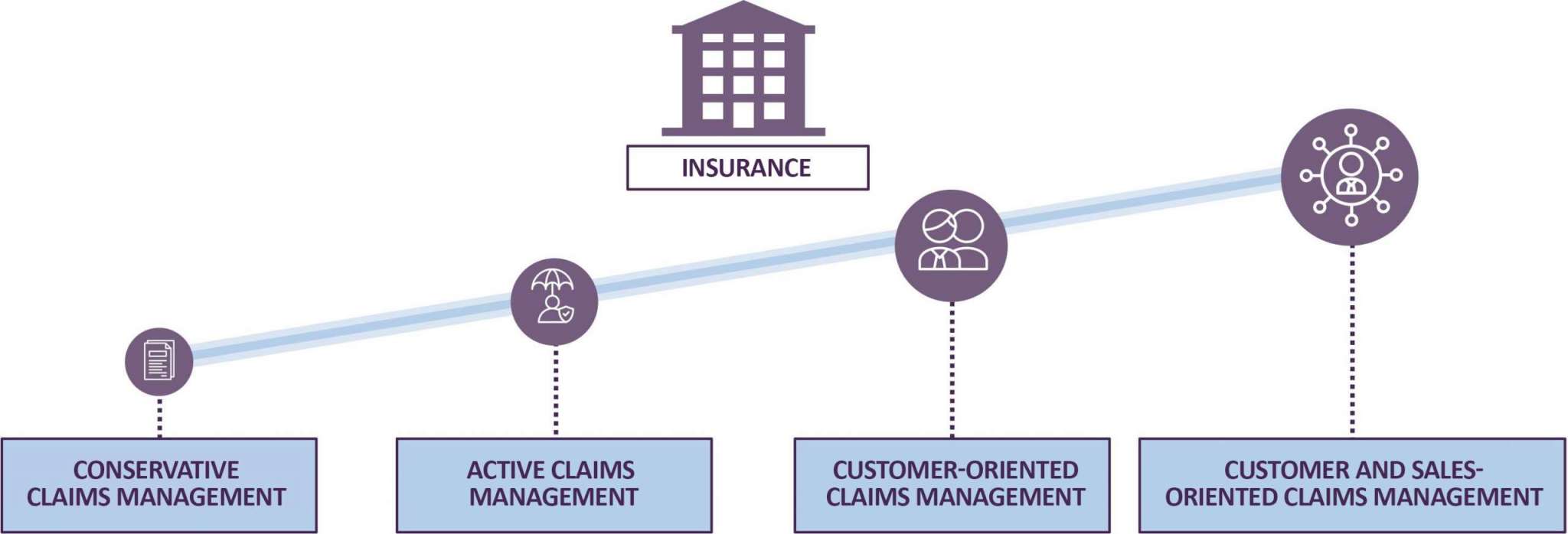
Reporting a damage is equivalent to starting a crime movie. The damage event in real life represents the crime in the crime thriller. Throughout the film, the viewer is now provided with the information he or she needs to gradually discover the solution to the crime – including the perpetrator, motive and the exact execution. For an insurance customer who suffers a loss, this flow of information would be ideal in contrast to the opaque claims handling process found in insurance companies today. A film whose trailer is spectacular and goes straight to the credits should not receive much positive criticism. In the entire film, however, the viewer is taken on a journey and can experience the suspense. If, however, only the claim notification (trailer) and the credits (final claim notification) are recognizable as process steps for the customer, the criticism for the director and the insurer should be similar. This is exactly where insurers need to start and rethink. Why don’t I make the individual internal process steps transparent to my customer? Active claims management is the magic word. The customer is happy to receive reliable information. After all, the uncertainty caused by missing information does not exactly strengthen the relationship of trust between customer and insurer.
In practice, approaches of active claims management are already a common practice, such as the mediation to a service provider (e.g. workshop) with the request to organize an appointment independently. The customer orientation must be questioned here however. Wouldn’t it be great if the service provider would contact the customer as quickly as possible and independently? In this case, the insurer acts as a counterpart to the investigator in the crime thriller, who successively solves the case – be it the crime in the film or the insurance case. The insurance customer would thus be an active participant in the process – just like the viewer in a good feature film. Insurers are called upon to make processes transparently accessible to their customers in order to solve the case quickly and cost-effectively by joining forces.
Transparency as a success factor in claims management
Insurers have similar goals in mind. The TOP goals from the perspective of claims management are:
- Increase of customer satisfaction
- Reduction of claims payments
- Reduction of performance process costs
In a world where almost everything is available at any time, transparency and access to information is an essential success factor. If an insurer integrates the customer into claims processing, customer satisfaction is automatically increased. The affected party becomes a participant. Service process costs can thus be optimized by reducing the number of queries. The integration of the claimant can also reduce claims payments, as the provision of services no longer acts as paternalism on the part of the insurer.
However, the customer’s journey begins even before the damage occurs. Supportive prevention measures by insurers help the customer to avoid damage even before it occurs. The standardized claims process is therefore not sufficient for customer orientation. The intelligent use of data and technology will play a decisive role for insurers. For example, storm and hail warnings could help prevent damage to buildings and motor vehicles. However, the dishonest customer may well sense his or her chance of fraud here and explicitly place his or her vehicle in the storm in the event of hail. The prevention service of the insurer is similar to the trailer of a feature film. The fight against insurance fraud through fraud management could even become a thriller.
Can we support you? Contact our experts!
With WAVESTONE, you have a strong partner at your side.
We look forward to your challenge!